There is worrying evidence that certain bacteria are becoming resistant to antibiotics. Mark Bowen MRCVS discusses the repercussions
Modern veterinary medicine depends upon antibiotics to treat persistent infections and to prevent the formation of disease-causing bacteria in wounds and surgical sites.
The harsh reality is that some antibiotics are not working as well as they used to. We can no longer take it for granted that they will clear up bacterial illness, as the story in Horse & Hound last week about eventer Trig Point’s battle with a multiple-resistant bacterial infection proved.
The problem of antibiotic resistance, already described as one of the biggest threats facing human health, is rapidly becoming an issue in the equine world. But what exactly is happening — and why?
Q Are all bacteria bad?
Bacteria are everywhere in the environment. The majority are commensal, living on or in an animal without causing any harm.
The large colon (intestine) of the horse is full of commensal bacteria that help to digest plant material. Furthermore, commensal bacteria make growth conditions for disease-causing (pathogenic) bacteria difficult, by competing for nutrients or changing the environment in which they live. As such, commensal organisms can protect us from disease and are sometimes referred to as “good bacteria”.
A second type of bacteria is referred to as opportunistic. These bacteria are not predominantly pathogenic but, given the right circumstances (such as tissue injury), can multiply rapidly and cause injury to their host. Pseudomonas aeruginosa is an example of an opportunistic bacterium — when it contaminates a wound it can cause severe disease.
Pathogenic bacteria include strangles and salmonella. In some cases a horse may become a silent carrier of these bacteria, able to limit their growth, although infection can reoccur if the bacteria are given an opportunity to multiply again. This may happen if:
• The immune system is not functioning.
Stress, severe disease, some medicines and equine Cushing’s disease can all impact on a horse’s ability to fight infection naturally.
• Competition from commensal bacteria is removed.
Removal of good bacteria by the use of antibiotics can allow pathogenic bacteria to flourish and grow. A reduction in intestinal commensal bacteria can result in severe diarrhoea due to overgrowth of pathogens.

Q How does antibiotic resistance occur?
Antibiotics either directly kill bacteria (when they are termed bactericidal), or stop them from growing so that ultimately the animal’s own immune response can control the infection (bacteriostatic). They may be classified as “broad spectrum”, killing many different bacteria, or “narrow spectrum”, meaning that only a small proportion of bacteria will be susceptible to their effects.
Resistance occurs when a population of bacteria is no longer susceptible to a previously effective antibiotic. For this to happen, the genetic code of a bacterium must change so that it is protected from the action of the antibiotic. The code can change by spontaneous mutation or through acquisition of genes from other bacteria.
Evolution then takes over to ensure survival of the fittest. If mutation provides the cell with a benefit, it will multiply and eventually become the dominant form.
Where mutation brings about bacterial resistance and the bacteria are not exposed to antibiotics, numbers of these newly resistant bacteria will remain small. The use of antibiotics, however, can kill off normal bacteria and allow the resistant ones to take over.

Q What is a superbug?
The term “superbug” is sometimes given to resistant bacteria, but it can be misleading. These bacteria are no more dangerous than they would be without the genetic code for resistance — resistance does not mean “flesh-eating”.
The most well-known resistant bacteria is MRSA (methicillin resistant Staphylococcus aureus), which causes infection of wounds or injection sites. The body’s immune mechanism will still mount a response to this bacteria, and, in most cases, some of the newer antibiotics will be effective.
In veterinary medicine there are currently very few bacteria that cannot be defeated by any antibiotic.
If this situation escalated, however, we would struggle to manage such infections.
This apocalyptic “post-antibiotic” era may be some way off, but scientists have not developed a new class of antibiotic in almost 30 years. Many medical professionals believe that a world without effective antibiotics is inevitable.
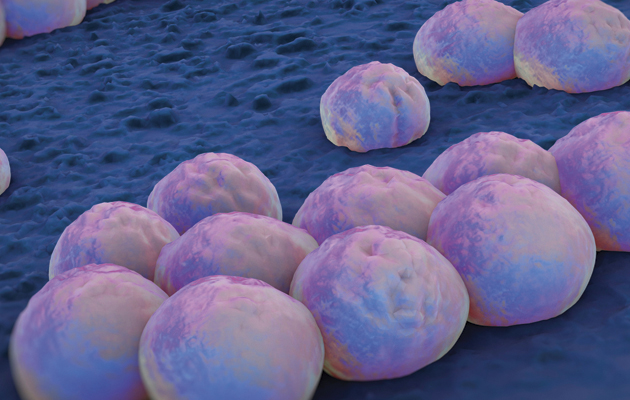
Clusters of ‘superbug’ (MRSA) bacteria
Q What happens if my horse develops an infection caused by resistant bacteria?
Pseudomonas, the bacteria that populated Trig Point’s sinuses, is normally only susceptible to a small range of antibiotics. When resistance occurs, the remaining available antibiotics become very limited.
To determine which antibiotic will be effective, a bacterial sample is grown in the laboratory and tested against multiple antibiotics.
If no such drug is available then other methods need to be employed to limit bacterial growth until the horse is able to mount his own immune response. Options may include surgery to debride (cut away) infected tissue or lavaging to flush out bacteria. Topical antiseptic solutions may be used where possible.
Q What is being done to prevent resistance?
Attempts to invent and discover new antibiotics are vital, but they’re not the whole answer.
It is essential that antibiotics are used carefully and only when necessary. Most UK equine vets have signed up to the Protect ME policy developed by the British Equine Veterinary Association (BEVA). This aims to reserve antibiotics defined as critically important for both animal and human health, so that they are used only for cases where they are genuinely required.
It is also important that vets and horse owners comply with guidelines for responsible antibiotic use.
Through such methods it is hoped that these medicines will remain effective for as long as is possible.
Ref: Horse & Hound; 24 September 2015
